A 70 year old with loin pain
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based inputs.
This E log book also reflects my patients-centered online learning portfolio and your valuable inputs on the comment box is welcome.
CASE;
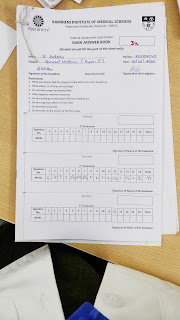
E.Likhitha
8th sem
Roll no.43
A 70 year old female,resident of Erupu village of suryapet district,home maker by occupation came to the hospital with,
C/O,
Loin pain on Right side since 3 years.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 3 years back and then she developed loin pain on right side,pricking type ,which is insidious in onset and gradually progressive .
Then she developed fever from 2 years associated with chills and on medication from 2 years ,it subsides after taking and again regains after sometime.
H/O shortness of breath from 3 years which is of Grade-4 ,breathlessness during resting position
H/O vomitings from 3 months which is of 2 episodes per day and 3 times per week .
Hypertension was diagnosed at the date of admission on (22-12-22).
No H/O low urine output ,burning micturition,pedal edema.
PAST HISTORY:
No similar complaints in the past .
No H/O diabetes ,hypertension,coronary artery disease,seizures and epilepsy.
H/O fall 4 years back for which she underwent a surgery
PERSONAL HISTORY:
Routine history : she wakes up at 6 am in the morning and eats breakfast ,then lunch at 1pm and dinner at 8pm,sleeps at 10-11 pm.She unable do her routine works, so her husband is taking care of her.
Diet-mixed
Appetite-decreased appetite
Sleep-adequate
Bowel and bladder movements -Regular
Addictions - none
FAMILY HISTORY:
No significant family history
DRUG HISTORY:
Tab.Paracetamol since 2 years(2-3 pills per day).
GENERAL EXAMINATION:
Patient was conscious,coherent and cooperative and well-oriented to time ,place,person.Moderately built and nourished.
Pallor present
No icterus
No cyanosis
No clubbing
No generalized lymphadenopathy
No edema
VITALS:
Temperature-febrile
BP:130/80mmHg
RR:20cpm
PR:80bpm
SYSTEMIC EXAMINATION:
Cardiovascular system-S1 and S2 are heard ,no murmurs present.
Respiratory system-Trachea central and normal vesicular breath sounds are heard.
Central nervous system-no neurological deficits
Per abdomen- soft ,non tender ,no organomegaly.
Inspection:
On inspection abdomen is flat, symetrical,and slightly distended.
Umbilcus is centre and inverted
No scars,engorged veins are seen.
All 9 regions of abdomen are equally moving with respiration.
Palpation:
On palpation abdomen is soft and non tender
.On bimanual examination of kidney is not palpable.All inspectory findings are confirmed.
Percussion:no shifting dullness, no fluid thrills
.
Auscultation:normal bowel sounds are heard.
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS:
CKD with Denovo hypertension with NSAID abuse
TREATMENT:
Fluid restriction
Salt restriction
Inj.LASIX- 40mg IV -TID
Inj.REPOITIN -4000 IV/Weekly once subcutaneously
Tab.SHELCAL- 500mg OD Per orally
Tab.SOBOSIS FORTE -1gm TID Per orally
Tab.Nicardia-10mg per orally
Nebulizer with SALBUTAMOL 6th hourly
Potassium bind sachets in one glass of water per oral TID
Syrup.CREMAFFIN -10ml per oral
Capsule.BIO D3-Per oral OD weakly once
Tab.ULTRACET -1/2 tab QID
Inj.ZOFER-4mg IV TID.














Comments
Post a Comment