A 55 year old with shortness of breath since 2 days
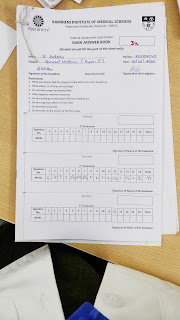
E.Likhitha
Roll no.34
A 55 year old male ,who is a toddy maker by occupation and residency of chotuppal ,came to the department with ,
C/O Shortness of breath since 2 days
Fever since 2 days
Cough since 1 day.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 3 years back ,then he developed shortness of breath of Grade-2 (acc. to MMRC ) the patient cannot walk beyond 500m and as he was a toddy maker ,he develops SOB on uphill,which is insidious in onset and not progressed till 10-04-23 and it is not associated with orthopnea and paroxysmal nocturnal dyspnea ,aggravated on exposure to cool temperature,by eating sweet and sour food,on exposure to dust in traffic and it is relieved on medication .
On 10-04-23,patient developed SOB of Grade-4(acc.to MMRC),he developing SOB even at rest ,which is sudden in onset and non progressive associated with wheeze ,due to this he was admitted in hospital .
Dry cough occasionally from past 3 yrs on exposure to cool temperature,eating sweets and exposure to dust and it relieved on medication.
H/O fever since 2 days ,which is insidious in onset ,intermittent in nature not associated with chills and rigors and it is relieved on medication .
H/O cough since 1 day ,which is dry and not associated with sputum,it is of 2 episodes and each episode had 10-12 bouts ,aggravated on exposure to cool temperature and relieved on medication .
No H/O chest pain,chest tightness,haemoptysis,
No H/O nausea,vomitings.
PAST HISTORY :
H/O asthma since 3 years ,for that he is using inhalers (composed of bronchodilators and corticosteroids),till now he changed his medication only once , inhaler usage 2 times per day and at each usage 3 puffs taken.
No H/O DM,TB,HTN,epilepsy,CAD.
No similar complaints in the past .
PERSONAL HISTORY:
Diet-mixed
Appetite-normal
Sleep-regular
Bowel and bladder movements - regular
Addictions-he is a chronic smoker since 25 years 1 pack per day,and stopped since 5 years.
.Alcohol occasionally
FAMILY HISTORY:
No significant family history.
DRUG HISTORY:
He is on medication for asthma since 3 yrs (bronchodilators +corticosteroids).
GENERAL EXAMINATION:
Patient is conscious ,coherent and cooperative and moderately built and nourished.
No signs of pallor,icterus,cyanosis,clubbing,generalized lymphadenopathy,pedal edema.
Vitals: temperature-afebrile
BP-120/80mmHg
RR-26cpm
PR-72bpm
RESPIRATORY EXAMINATION :
INSPECTION:
Upper respiratory tract-Nose: No polyps,DNS,turbinate hypertrophy
Oral cavity:No dental caries,normal oral hygiene ,no halitosis,post nasal drip and normal posterior pharyngeal wall.
Lower respiratory tract:
Shape of chest-elliptical.
Trachea seems to be central
Chest movements appears to be equal on both side. Apex beat not seen visually
No drooping of shoulders
No crowding of ribs
Usage of accessory muscles of respiration are normal
No kyphosis,scoliosis,supraclavicular hallowing,intercoastal indrawing and widening,pectus excavatum ,pectus carinatum
No scars,sinuses over chest.
PALPATION:
No local rise of temperature and tenderness over chest.
Trachea - central
Chest movements are equal on both sides
Chest expansion is normal
On inspiration-87cm
On expiration -85cm
Antero-posterior diameter-28cm
Transverse diameter-32cm
Apex beat not felt properly
Vocal fremitus - normal on all areas.
PERCUSSION:
Dull note heard on left side of chest on Mammary area.
Remaining ,supraclavicular area,infraclavicular area,mammary area(right),axillary area,infra axillary area,supra scapular area,infra scapular area,inter scapular area.
AUSCULTATION:
Bilateral rhonci heard on Mammary area,infra axillary area,suprascapular area and infra scapular area
Remaining areas are normal.
CVS EXAMINATION:
S1 S2 heard,no murmurs
JVP not raised
Apex beat not felt properly
PER ABDOMEN EXAMINATION:
soft ,non tender,no organomegaly present.
CNS EXAMINATION:
No neurological deficits .
PROVISIONAL DIAGNOSIS.
Obstructive respiratory disease.
INVESTIGATIONS:
FINAL DIAGNOSIS:
Obstructive respiratory disease.
TREATMENT:
O2 inhalation with face mask 4-6lit/min to maintain spo2-95
Syp.GRILLINCITUS TID
Inj.PIPTAZ 4-5gm IV TID
Tab.PANTOP 40mg
Tab.SHELCAL OD
LIDILIV 300mg BD
Inj.HYDROCORT 100mg 2hrs after meal.




Comments
Post a Comment